ADOS Testing
How ABA Therapy Can Help Kids
If you have more questions about how our Fort Myers ABA therapy team can help your child, contact us! FOCUS Therapy offers ABA therapy and ADOS testing to children in Lee County, Florida. Call (239) 313.5049 or Contact Us online.
- Categorized: ABA Therapy, ADOS Testing
FOCUS Therapy Only Schedules Evaluations if We Have Space to Treat Your Child
Evaluations are an important step in the process of securing speech, occupational, physical, and/or ABA therapy for your child. But parents and caregivers should be wary of facilities that offer these evaluations while lacking capacity to immediately treat the child.…
- Categorized: ABA Therapy, ADOS Testing, Occupational Therapy, Speech Therapy
- Tagged: FOCUS ABA therapy, FOCUS speech therapy, Focus Therapy, FOCUS Therapy Fort Myers, Fort Myers ABA Therapy, Fort Myers ADOS testing, Fort Myers speech therapy, Lee County ADOS testing, Lee County pediatric speech therapy, Southwest Florida ADOS testing
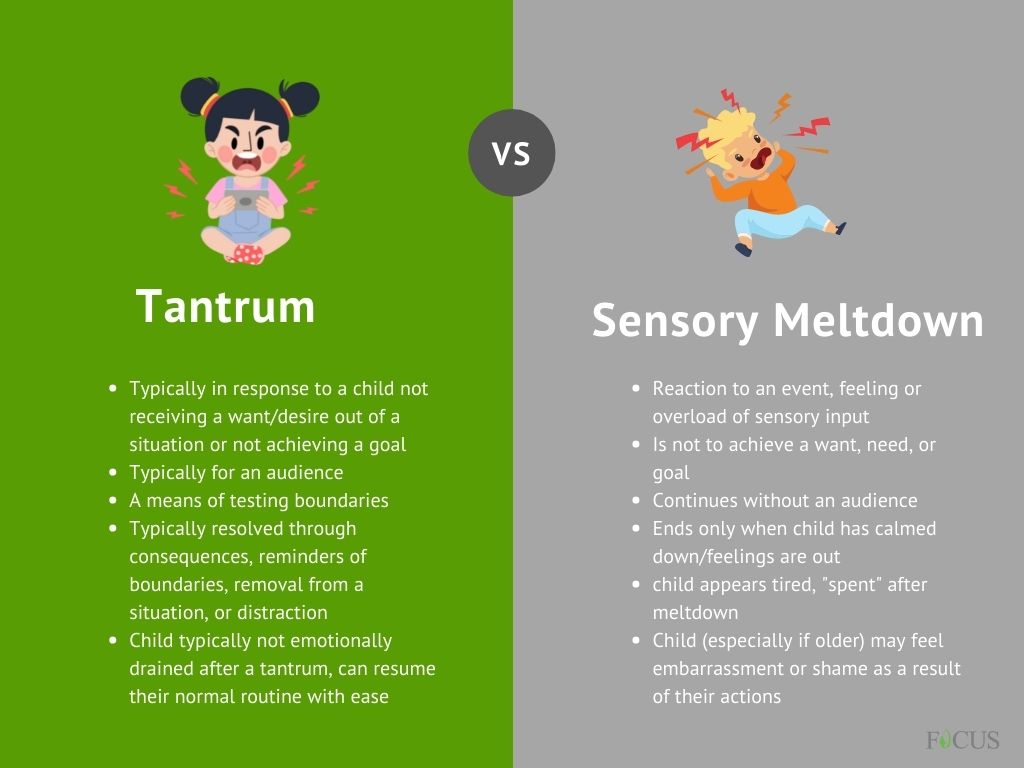
Tantrum or Sensory Meltdown? Fort Myers ABA Therapists Explain
When working with kids who have varying sensory struggles, it can be difficult to tell the difference between a tantrum or a sensory meltdown. Our Fort Myers ABA therapists recognize that it often takes some detective work to differentiate. But…
- Categorized: ABA Therapy, ADOS Testing, Behavior Therapy
- Tagged: behavior therapy, child tantrums, Fort Myers ABA, Fort Myers ABA Therapy, sensory meltdown
Study: Less than 1/2 Kids With Autism Undergo Early Intervention Therapy
Early intervention therapy for autism is crucial to optimal long-term outcomes for children on the spectrum. “Early intervention,” defined as a combination of speech therapy, occupational therapy, physical therapy, nutrition/feeding therapy, and ABA therapy, should ideally begin before age 3…
- Categorized: ABA Therapy, ADOS Testing
- Tagged: Autism diagnosis, early intervention Fort Myers, Early intervention therapy, Florida early intervention therapy, Fort Myers autism diagnosis, Fort Myers early intervention, Fort Myers early intervention therapy, Lee County ADOS testing, Lee County autism treatment, Lee County early intervention, Lee County occupational therapy, Lee County speech therapy, Southwest Florida autism, Southwest Florida autism diagnosis, Southwest Florida autism resources
5 Steps to ABA Therapy in South Florida
ABA therapy is considered the gold standard treatment for kids with autism spectrum disorder (ASD). But the process of starting this therapy is not as simple as calling and setting an appointment. There are several steps that must be taken…
Why FOCUS Asks Parents to Stay in the Waiting Room During Evals, Sessions
FOCUS Therapy in Fort Myers conducts a range of in-depth evaluations for children who have been referred for speech, occupational, physical, or ABA therapies as well as ADOS testing. During our evaluations and therapy sessions, we rarely allow families to…
- Categorized: ABA Therapy, ADOS Testing, FOCUS News, Speech Therapy
- Tagged: ABA therapy, Bonita Springs ADOS testing, Bonita Springs speech therapy, Cape Coral ADOS testing, Fort Myers ABA Therapy, Fort Myers ADOS testing, Fort Myers kids speech therapy, Fort Myers speech therapy, Lehigh Acres ADOS testing, Lehigh Acres speech therapy, occupational therapy, physical therapy, Southwest Florida ADOS testing, Southwest Florida speech therapy, speech therapy
Study: ADOS Testing Measures Autism Risk Equally Well in Boys and Girls
ADOS testing, also known as the Autism Diagnostic Observation Schedule, was found in a recent, large study to measure severity of autism traits equally well in both girls and boys. This is good news because research has shown doctors may…