Occupational Therapy
Fort Myers Occupational Therapists Explain Sensory Diet
- Categorized: Occupational Therapy
- Tagged: Fort Myers occupational therapy, occupational therapy
“Heavy Work” Recommended by Fort Myers Occupational Therapists
“Heavy work” can go a long way toward helping kids self-regulate – which also minimizes tantrums and emotional outbursts. Check out some of the “heavy work” activities recommended by our Fort Myers occupational therapists.
- Categorized: Occupational Therapy
- Tagged: Fort Myers occupational therapy, occupational therapy
Fort Myers Swimming Lessons Can Reduce Drowning Risk for Kids With Disabilities
Children with disabilities are often at higher risk of drowning, particularly in Florida. Fort Myers swimming lessons can go a long way toward reducing that risk. A few local Fort Myers swimming lessons providers that may be helpful resources for…
- Categorized: Occupational Therapy
- Tagged: Fort Myers occupational therapy, occupational therapy
“Occupational Therapy for Babies? What Does That Look Like?”
At FOCUS Therapy, we heavily gear many of our occupational therapy efforts toward early intervention. That means for certain conditions and especially those with developmental delays, the sooner we start, the better – because we can more effectively “train” neural…
- Categorized: Articles, Occupational Therapy
- Tagged: Fort Myers occupational therapy, occupational therapy
Fort Myers Occupational Therapy Helps Kids Acquire Life Skills
When parents first learn their child has been referred to Fort Myers occupational therapy raise an eyebrow. After all, what “occupation” does a child have? The answer is: Many! But we have to look beyond the traditional definition of “occupation,”…
- Categorized: Occupational Therapy
- Tagged: Fort Myers occupational therapy, occupational therapy
Fort Myers OT Explains In-Clinic vs. School-Based
- focustherapy
- Jan 05, 2024
- Comments: ( 1 )
If your child has been referred to pediatric occupational therapy services, you may be wondering what’s the point of getting both in-clinic occupational therapy AND school-based occupational therapy. As a Fort Myers OT can explain, these are often similarly-qualified professionals…
- Categorized: Occupational Therapy
- Tagged: Fort Myers occupational therapy, occupational therapy
Improving Executive Functioning Skills for Kids is Often a Top Therapy Goal
As our Fort Myers pediatric therapists can explain, improving executive functioning skills for kids is one of the most common goals listed in our patients’ plans of care. That’s because these skills play a crucial role in a child’s overall…
Fort Myers Occupational Therapy Tips for Maximum Attention & Listening
Is your child always “buzzing” off-the-walls? To maximize attention & listening, try these Fort Myers occupational therapy tips. They can be especially helpful for kids who are neurodivergent, language delayed, or diagnosed with conditions like attention deficit hyperactivity disorder (ADHD).…
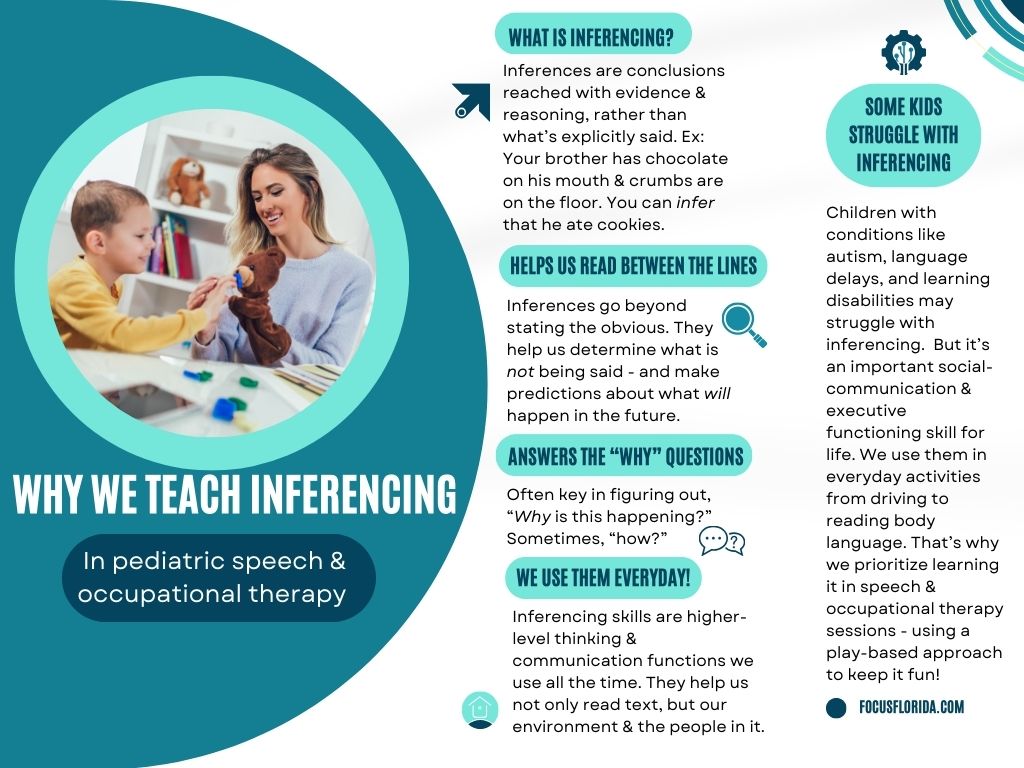
Why Occupational & Speech Therapists in Fort Myers Teach Kids Inferencing
Inferencing is often thought of as a “school skill.” But as our occupational & speech therapists in Fort Myers can explain, it’s one that starts to develop long before kindergarten and has far more applications than a language arts class.…